Ponstel
By G. Grimboll. North Carolina Central University. 2019.
Serological screening to identify susceptibles is impractical and unnecessary buy ponstel 500mg, since there is no risk in immu- nizing those who are already immune purchase ponstel 250mg otc. Identification—An acute viral disease characterized by paroxysmal spasmodic pain in the chest or abdomen, which may be intensified by movement, usually accompanied by fever and headache. The pain tends to be more abdominal than thoracic in infants and young children, while the reverse applies to older children and adults. Most patients recover within 1 week of onset, but relapses occur; no fatalities have been reported. It is important to differentiate from more serious medical or surgical conditions. Complications occur infrequently and include orchitis, pericarditis, pneumonia and aseptic meningitis. During outbreaks of epidemic myalgia, cases of group B coxsackievirus myocarditis of the newborn have been reported; while myocarditis in adults is a rare complication, the possibility should always be considered. Diagnosis is suggested by the appearance of similar symptoms among multiple family members; it is confirmed by a significant rise in antibody titre against specific etiologic agents in acute and convalescent sera, or isolation of the virus in cell culture or neonatal mice from throat secretions or patient feces. Infectious agents—Group B coxsackievirus types 1–3, 5 and 6, and echoviruses 1 and 6 are associated with the illness. Many group A and B coxsackieviruses and echoviruses have been reported in sporadic cases. Occurrence—An uncommon disease, occurring in summer and early autumn; usually in children and young adults aged 5–15, but all ages may be affected. Mode of transmission—Directly by fecal-oral or respiratory drop- let contact with an infected person, or indirectly by contact with articles freshly soiled with feces or throat discharges of an infected person who may or may not have symptoms. Group B coxsackieviruses have been found in sewage and flies, though the relationship to transmission of human infection is not clear. Period of communicability—Apparently during the acute stage of disease; stools may contain virus for several weeks. Susceptibility—Probably general; type-specific immunity presum- ably results from infection. Control of patient, contacts and the immediate environment: 1) Report to local health authority: Obligatory report of epidem- ics, Class 4 (see Reporting). Because of possible serious illness in the newborn, if a patient in a maternity unit or nursery develops an illness suggestive of enterovirus infection, precautions should be instituted at once. Individuals with suspected enterovirus infections (in- cluding health personnel) should be excluded from visiting maternity and nursery units and from contact with infants and women near term. Careful attention must be given to prompt, thor- ough handwashing when handling discharges, feces and articles soiled therewith. Epidemic measures: General notice to physicians of the presence of an epidemic and the necessity for differentiation of cases from more serious medical or surgical emergencies. Identification—A clinical syndrome caused by a variety of aerobic actinomycetes (bacteria) and eumycetes (fungi), characterized by swelling and suppuration of subcutaneous tissues and formation of sinus tracts with visible granules in the pus draining from the sinus tracts. Lesions are usually on the foot or lower leg, sometimes on the hand, shoulders and back, and rarely at other sites. Mycetoma may be difficult to distinguish from chronic osteomyelitis and botryomycosis (a clinically and pathologically similar entity caused by a variety of bacteria, including staphylococci and Gram-negative bacteria). Specific diagnosis depends on visualizing the granules in fresh prepara- tions or histopathological slides and isolation of the causative actinomy- cete or fungus in culture. Occurrence—Common in Mexico, Africa, southern Asia and other tropical and subtropical areas, especially where people go barefoot. Mode of transmission—Subcutaneous implantation of conidia or hyphal elements from a saprophytic source by penetrating wounds (thorns, splinters). Susceptibility—Causal agents are widespread in nature, but clinical infection is rare, which suggests intrinsic resistance. Preventive measures: Protect against puncture wounds by wearing shoes and protective clothing. Control of patient, contacts and the immediate environment: 1) Report to local health authority: Official report not ordinarily justifiable, Class 5 (see Reporting). Resection of small lesions may be helpful; amputation may be required for an extremity with advanced lesions. In suspected Acanthamoeba infections, diagnosis is made by microscopic examination of scrapings, swabs or aspirates of the eye and skin lesions; or by culture on nonnutrient agar seeded with Escherichia coli, Klebsiella aerogenes or other suitable Enterobacter species. Amoebae have been misidentified as macrophages and have been mistaken for Entamoeba histolytica when microscopic diagnoses are made under low magnification. Reservoir—Acanthamoeba and Naegleria are free-living in aquatic and soil habitats.
Although transmission from a patient to attending personnel has not been documented buy discount ponstel 500mg, immediate attendants should be warned of the potential hazard of infection from saliva buy 250mg ponstel otc, and wear rubber gloves, protective gowns, and pro- tection to avoid exposure from a coughing patient. Epidemic (epizootic) measures: Applicable only to animals; a sporadic disease in humans. For protection of other domes- tic animals, use approved vaccines appropriate for each animal species. Disaster implications: A potential problem if the disease is freshly introduced or enzootic in an area where there are many stray dogs or wild reservoir animals. International measures: 1) Strict compliance by common carriers and travellers with national laws and regulations in rabies-free countries. Immu- nization of animals, certificates of health and origin, or microchip identification of animals may be required. Vaccination Status Treatment Regimen* Not previously Wound All postexposure treatment to begin with immediate vaccinated cleansing thorough cleansing of all wounds with soap and water. If available, a virucidal agent such as a povi- done-iodine solution should be used to irrigate the wounds. Previously Wound All postexposure treatment to begin with immediate vaccinated§ cleansing thorough cleansing of all wounds with soap and water. If available, a virucidal agent such as a povi- done-iodine solution should be used to irrigate wounds. Strepto- bacillosis is caused by Actinobacillus muris (formerly Streptobacillus moniliformis or Haverhillia multiformis) and spirillary fever or sodoku by Spirillum minus (minor). Because of their clinical and epidemiological similarities, only streptobacillosis is presented in detail; variations mani- fested by Spirillum minus infection are noted in a brief summary. Identification—An abrupt onset of chills and fever, headache and muscle pain, is followed within 1–3 days by a maculopapular rash most marked on the extremities. There is usually a history of a rat bite within the previous 10 days that healed normally. Bacterial endocarditis, peri- carditis, parotitis, tenosynovitis and focal abscesses of soft tissues or the brain may occur late in untreated cases, with a case-fatality rate of 7%–10%. Laboratory confirmation is through isolation of the organism by inocu- lating material from the primary lesion, lymph node, blood, joint fluid or pus into the appropriate bacteriological medium or laboratory animals (guinea pigs or mice that are not naturally infected). Occurrence—Worldwide, but uncommon in North and South America and most European countries. Mode of transmission—Urine or secretions of mouth, nose or conjunctival sac of an infected animal, most frequently introduced through biting. Direct contact with rats is not necessary; infection has occurred in people working or living in rat-infested buildings. In outbreaks, contaminated milk or water has usually been suspected as the vehicle of infection. Control of patient, contacts and the immediate environment: 1) Report to local health authority: Obligatory report of epidem- ics in most countries; no case report required, Class 4 (see Reporting). Epidemic measures: A cluster of cases requires search for a common source, possibly contaminated food and water. Clinically, Spirillum minus disease differs from streptobacillary fever in the rarity of arthritic symptoms and the distinctive rash of reddish or purplish plaques. The incubation period is 1–3 weeks, and the previously healed bite wound reactivates when symptoms appear. Laboratory methods are essential for differentiation; animal inoculation is used for isolation of the Spirillum. Identification—A systemic louse-borne epidemic or tick-borne sporadic spirochaetal disease in which periods of fever lasting 2–9 days alternate with afebrile periods of 2–4 days; the number of relapses varies from 1 to 10 or more. Total duration of the louse-borne disease averages 13–16 days; usually longer for the tick-borne disease. Symptoms vary with host immunity, strain of Borrelia involved and phase of the epidemic. Neuropsychiatric symptoms are more common in tick-borne than in louse-borne epidemics. Predisposing factors (thiamine and vitamin B deficiency) may lead to neuritis or encephalitis. Severity varies according to individual susceptibility (in Africa infections are severe for Europeans but milder for the local population) and to geography (tick-borne infec- tions may be severe in Egypt, Israel, Lebanon, the Syrian Arab Republic, Pakistan and mild in Poland, Romania and the Russian Federation). Diagnosis is made during the attack through demonstration of the infectious agent in darkfield preparations of fresh blood or stained thick or thin blood films, through intraperitoneal inoculation of laboratory rats or mice with blood taken during the febrile period or through blood culture in special media. Infectious agents—In louse-borne disease, Borrelia recurrentis,a Gram-negative spirochaete. In tick-borne disease, different strains have been distinguished by area of first isolation and/or vector rather than by inherent biological differences. Strains isolated during a relapse often show antigenic differences from those obtained during the immediately preceding paroxysm.
When junction opens to receive the bolus which is the bolus has passed further down the oeso- pushed down by contraction of the circular phagus discount 250mg ponstel with visa, the pressure in the pharyngo- muscles of the pharynx purchase ponstel 250mg on-line. This is due to dehydration causing decrea- Two sounds can be heard on auscultation over sed salivary secretion and drying of the the oesophagus during swallowing. Impulses from those receptors the commencement of the act and is prob- are conducted along fibres in the ninth and ably due to the fluids impinging on the tenth nerves. The second sound resembles a bubbling or secretion or by local anaesthesia of the trickling noise and occurs at a variable interval of 4-10 seconds after the first sound pharyngeal mucous membrane. In drive” is supposed to be the central compo- recumbant subjects the second sound is nent (not agreed by all). It seems to be replaced by a few discrete squirting related to intracellular osmolarity. When Intravenous hypertonic saline or a high a solid bolus is swallowed, the second intake of salt with low water intake, sound may be absent. This osmotic The sensation of thirst is composed of two effect acts on the osmoreceptor neurons in components. Pain from the oropharyngeal diseases may be referred to the ear (referred otalgia). This can result from a variety of lesions in the oral Difficulty in Respiration cavity, pharynx and oesophagus (Fig. Trauma, tumours and infections can lead to The lesions could be inflammatory, paralytic airway obstruction. Regurgitation occurs in paralytic lesions of the soft palate when the ingested Palatal paralysis or sometimes adenoidectomy material regurgitates into the nose. Paralysis lead to improper closure of the nasopha- of the pharynx may lead to dysphagia as well ryngeal isthmus with resulting hypernasality as to aspiration into the trachea. This the anterior two-thirds of the tongue for defect is called rhinolalia clausa. It should not be put on posterior-third of the tongue to avoid Ulceration of Pharyngeal Mucosa gagging. Surface of the hard and soft palate is Ulceration of the pharynx may be manifes- noted for any clefts, ulcers or tumour. The postnasal discharge which indicates a Cervical Lymphadenopathy nasal disease is seen trickling behind the soft palate. This may be the cause for many Enlargement of the cervical nodes is com- pharyngeal symptoms. The posterior pharyn- monly due to infective or neoplastic lesions geal wall is seen bulging in case of retro- of the oral cavity, pharynx, larynx and pharyngeal abscess. The patient is asked to open the mouth and an inspection Palpation of the oral vestibule is done. The Finger palpation is necessary to examine the patient is asked to lift the tip of the tongue inside of the oral cavity and pharynx and and orifices of the submandibular ducts and should be routinely done. Movements of the mouth) and that of the floor of the mouth is tongue are noted for paralysis or neoplastic necessary for evaluating the extent of a infiltration. Palpation of the tonsils Faucial pillars and condition of the tonsils and base of the tongue is necessary to diagnose are noted. Pressure by the tongue depressor certain infiltrative growths which may not squeezes the debris from the tonsillar crypts show on the surface. The colour of the mucosa, process may be felt on palpating through the ulcerations and membrane formation are tonsillar fossa. Palpation of the neck for lymph looked for in the oropharyngeal and buccal nodes forms an essential part of the mucosa. Common Symptoms of Oropharyngeal Diseases 251 Investigations Radiological Investigation Haematological Tests A plain X-ray of the neck (lateral view) provi- des clues for evaluating pharyngeal diseases. Like haemoglobin estimation total and X-ray of the chest, lateral view of the naso- differential counts are particularly required in pharynx, X-ray of the mandible are the other ulcerations of the oral cavity and oropharyn- views which may prove useful. Some of the common diseases of titis can be caused by staphylococcal, otolaryngologist interest are described here. Stomatitis is a general term for diffuse inflam- The infection is common in debilitated mation of the mouth. Inflammation of the oral patients, marasmic children and patients mucosa can be caused by local and systemic receiving broad-spectrum antibiotics. These Local Causes patches may coalesce to form a membrane Traumatic stomatitis The trauma may be due which can be removed. Diagnosis can be to ill-fitting dentures, hot foods, corrosives, confirmed by microscopical examination that simple cut of the mouth, too vigorous use of a show the fungal hyphae. The underlying debility Infective stomatitis Inflammation of the oral needs attention. Viral infections like herpes simplex or of this disease of unknown aetiology appear herpes zoster start as small painful vesicles as dull white or milky dots in a lace-like which later ulcerate, involving the lip, arrangement. Bacteria may produce inflammation like in Other local causes are the following: acute ulcerative stomatitis (Vincent’s i.
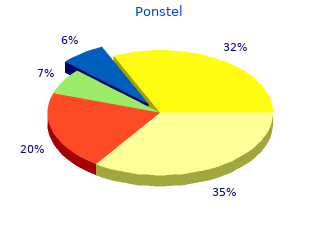
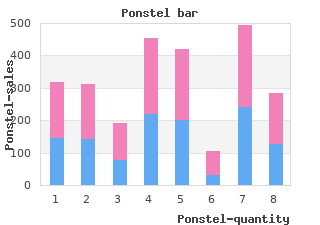
The percentage of outbreaks caused by a treatment deficiency and distribution system problem decreased relative to reported increases in the other three categories buy 500 mg ponstel with amex. The relative proportion and number of outbreaks associated with different water systems also differs from the figures from the 1997--1998 period (Figure 2) discount 500 mg ponstel free shipping. In addition, the number of outbreaks reported that were associated with individual systems during this period is the highest reported level since 1984. But noncommunity systems and individual systems, which are not regulated to the same extent, are continuing problems. The majority of these individual system outbreaks are linked to currently unregulated groundwater supplies, specifically private wells. The populations served by these systems merit increased attention by public health officials. These outbreaks of unknown etiology comprised the largest group of outbreaks, followed by outbreaks caused by bacteria (nine), parasites (seven), viruses (four), and chemicals (two). During 1997--1998, parasites accounted for the largest percentage of the 17 outbreaks (six [35. The number of outbreaks per type of agent were increased for all categories during 1999--2000, with the exception of chemicals. Although the number of reported viral outbreaks increased, indicating an improvement in the availability and usage of laboratory detection methods during previous years, viral outbreaks are probably substantially underreported. Although viruses were suspected in other outbreaks, specifically in those of unknown etiology, testing for viruses was not performed. The technology for detection of viruses in stool and water samples has improved, but testing for viruses is not widely practiced. Only two outbreaks of chemical origin were identified during this surveillance period, the same number as was reported during the 1997--1998 period. One outbreak related to a spill of sodium hydroxide at a community water treatment plant demonstrated the need for safe water treatment practices. The other outbreak was a single case of methemoglobinemia in an infant who required hospitalization after having been fed boiled water taken from a private well. Coordination of public health messages is critical; an intervention that was intended to reduce the transmission of infections agents concentrated the chemicals present in the water. These figures, as in the past, probably under represent the actual waterborne chemical poisonings that occur. Although no federal regulation exists for monitoring private wells, developing educational materials targeted towards the general public, informing them of ways to maintain the safety and water quality of their wells would be valuable. In addition, health messages regarding the consumption of nonpotable water and appropriate point-of-use treatment should be developed and distributed to the public. The 15 outbreaks reported in 1999 and 21 outbreaks reported in 2000 equal or surpass the number reported in 1998, which previously was the highest number of outbreaks involving recreational water-related gastroenteritis reported in one year since the inception of the surveillance system. Together, the outbreaks involving gastroenteritis reported during the 1999--2000 period are higher than the 18 outbreaks documented in the previous reporting period (Figures 7 and 8). Since 1989, the number of gastroenteritis- related outbreaks has been gradually increasing, and this increase is statistically significant (p = 0. Because swimming is essentially a shared water activity or communal bathing, rinsing of soiled bodies and overt fecal accidents cause contamination of the water. Unintentional ingestion of recreational water contaminated with pathogens can then lead to gastrointestinal illness, even in non-outbreak settings. Fresh and marine waters are also subject to other modes of contamination from point sources (i. Outbreaks involving gastroenteritis are more frequently observed during the swimming season, which usually starts on Memorial Day weekend (the last weekend in May) and ends Labor Day weekend (the first weekend in September). However, swimming also occurs year-round in indoor venues and in states with more temperate climates. Outbreaks of illness by month (Figure 3) include two outbreaks that occurred noticeably outside the summer months: one outbreak in a Florida pool in March and another outbreak in an indoor pool in Wisconsin in January. Waterborne Diseases ©6/1/2018 288 (866) 557-1746 As during the previous reporting period, Cr. However, the term treated system might pertain to systems not routinely treated, including wading pools, interactive fountains, and in one case, an untreated pool that was served by a natural hot springs source. Multiple interrelated factors can impede disinfection in treated venues, including an increased bather load in a pool, high levels of organic material (e. In certain outbreaks, fecal material was indicated on the report as a contributing factor to the outbreak; the majority of fecal accidents were attributed to young children who were in or near the water at the time the accident occurred. Unlike previous years, a substantial number of different bacterial and viral organisms were reported as causing gastrointestinal illness in these treated recreational water venues (Figure 9). Unlike other organisms, which are more susceptible to the levels of chlorine typically found in a pool, Cr. In addition, its relatively limited size (4--6 µm) can allow it to pass through particulate filtration systems during recirculation of water in the pool. Because a low number of oocysts might cause illness in a person, even ingestion of a limited amount of water can cause infection. The properties of the organism, coupled with the popularity of swimming and the tendency of persons to aggregate in larger water venues, increases the likelihood that swimming water can become contaminated and that swimmers will ingest the water and become infected.