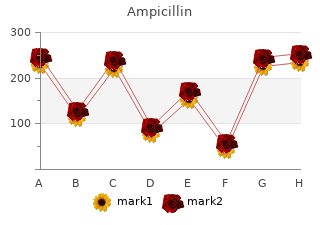
Ampicillin
By Y. Aila. Minnesota State University Moorhead.
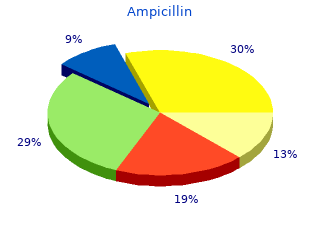
Incidence Commonest cause of emergency surgery of childhood Zollinger–Ellinson syndrome (3–4 per 1000) cheap ampicillin 500 mg without a prescription. Definition Pathological secretion of gastrin resulting in hypersecre- Age tion of acid buy ampicillin 500mg free shipping. Ultrasound is in- Aetiology/pathophysiology creasingly being used but does not exclude the diagnosis. Accumula- Conservative treatment has little place, except in patients tion of secretions result in distension, mucosal necrosis unfit for surgery. Fluid resuscitation may be required and invasion of the wall by commensal bacteria. Inflam- prior to surgery and intravenous antibiotics are com- mationandimpairmentofbloodsupplyleadtogangrene menced. Once perforation has occurred there is r Under general anaesthetic the abdomen is opened migration of the bacteria into the peritoneum (peritoni- by an incision along the skin crease passing through tis). Theoutcomedependsontheabilityoftheomentum McBurney’s point (one third of the distance from a and surrounding organs to contain the infection. The muscle fibres in each muscle layer Clinical features are then split in the line of their fibres (grid iron in- This is a classic cause of an acute abdomen. The mesoappendix is divided with ligation of tially periumbilical, then migrates to the right iliac fossa. The appendix is ligated at its There is mild to moderate fever, nausea and anorexia. The wound is then ment of the disease may be over hours to days partly closed in layers. In most cases, the appendix is tally particularly if the omentum is wrapped around the removed to avoid confusion if patients ever re-present appendix, or an abscess has formed. Macroscopy Prognosis The appendix appears swollen and the surface vascula- Uncomplicated appendicitis has an overall mortality of ture is yellow. Microscopy Meckel’s diverticulum Initially there is acute inflammation of the mucosa, which undergoes ulceration. As the condition progresses the inflammation An ileal diverticulum occurring as a result of persistence spreads through the wall until it reaches the serosal sur- of part of the vitellointestinal duct. Chapter 4: Disorders of the small bowel 165 Incidence due to ulceration of the adjacent ileum. Age Investigations Congenital Presence of gastric mucosa can be detected by scintiscan- ning with 99mTc labelled sodium pertechnetate, which is Sex taken up by parietal cells (the Meckel’s scan). Persistence of the Malabsorption syndromes ductmayresultinaMeckel’sdiverticulum(persistenceof Absorption of food occurs within the small bowel. The the ileal end of the duct), an umbilical sinus (persistence process involves breakdown of macromolecules by en- of the umbilical end of the duct) or an umbilical ileal zymes and transport across the specialised small bowel fistula (see Fig. The most common causes of Pathophysiology malabsorption are pancreatic insufficiency, coeliac dis- The diverticulum arises from the antimesenteric border ease, resection of the ileum, Crohn’s disease and liver of the ileum 2 ft from the ileocaecal valve and is on aver- disease (see Fig. Acid secreting gastric mucosa is found in 50% of cases which may result in Coeliac disease ulceration of the surrounding mucosa. Clinical features Ninety-five per cent of cases are asymptomatic, symp- Incidence tomatic patients present most commonly with bleeding 1in2000. There is lymphocytic infiltration of the lamina propria, and an increase in intra-epithelial lymphocytes (which Geography bear the γδ eceptor). Loss of normal villous architecture Common in Europe, (1 in 300 in Ireland) rare in Black ranges from blunting (partial villous atrophy) to com- Africans. Aetiology Investigations Thought to be an autoimmune disease with genetic and r Serology: Screening by IgG gliadin and IgG anti- environmental components. Management Clinical features Aglutenfree diet leads to a restoration of normal villous Patients may present with irritability and failure to thrive structure and resolution of dermatitis herpetiformis (see in childhood, delayed puberty, short stature, or vomit- page 394). Haemoglobin and antiendomysial antibodies ing, diarrhoea, anorexia or abdominal distension at any may be checked at routine follow-up to look for inad- age. Complications Whipple’s disease There is an association with development of small bowel lymphomaandasmallincreasedriskinthedevelopment Definition of small bowel adenocarcinoma. Chapter 4: Inflammatory bowel disease 167 Aetiology Disorders of the large bowel Caused by an infection by Tropheryma whippelii,anacti- and inflammatory bowel nomycete. Diverticular disease Clinical features Patients present with steatorrhoea, abdominal pain and Definition systemicsymptomsoffever,weightloss,lymphadenopa- Adiverticulum is a mucosal out-pouching, diverticular thy and arthritis. Investigations and management Incidence Electron microscopy can demonstrate the organism. Tropical sprue Definition Aetiology AseveremalabsorptionsyndromeendemicinAsia,some Diverticulae are associated with high intraluminal pres- Caribbean islands and parts of South America. There is a relationship with a low fibre diet and Aetiology/pathophysiology chronic constipation. The condition occurs in epidemics and improves on an- tibiotics thus it is likely that it has an infective cause.
However order ampicillin 500mg visa, there will be strategies for disease management that are additional to traditional management practices that once integrated purchase ampicillin 250mg visa, provide additional gains. To view disease management as separate to other forms of land and wildlife management ensures that opportunities for good disease prevention will be missed. Wetland managers are the key stakeholders in delivering healthy wetlands and, as such, all efforts should be made to integrate disease management thoroughly within wetland site management plans and other stakeholder activities at wetlands. Invasive alien species of flora and fauna are considered the second biggest threat after habitat loss and destruction to biodiversity worldwide, the greatest threat to fragile ecosystems such as islands, and are a major cause of species extinction in freshwater systems. Climate change may also exacerbate the spread of non-native species as warmer temperatures may allow currently ‘benign’ non-native species to potentially extend their ranges and become invasive. Invasive species impact native species in a wide range of ways, including competition, predation, hybridisation, poisoning, habitat alteration and disease. With respect to the latter, invasive alien species can carry novel pathogens non-symptomatically, to which native species may have no natural immunity. Crayfish plague], and amphibian chytridiomycosis carried non-symptomatically by introduced species such as American Bullfrogs Lithobates catesbeianus causes population declines and plays a role in amphibian extinctions [►Section 4. There are many parallels between prevention and control of invasive alien species, and of infectious diseases, such as the proactive measures of: Risk analysis and assessment ►Section 3. Communication, education, participation and awareness Training regarding management of those species ►Section 3. In general, to apply the concept of wise use and maintain biodiversity and ecological function i. Although a good understanding of disease dynamics is needed for the most effective proactive disease control strategies, there are some basic generic principles which, if implemented, are likely to reduce risks of disease emergence. For example, strategies for biosecurity (including prevention of introduction of invasive alien species), reduction of stresses on hosts and environment, and prevention of pollution, will bring obvious health benefits. Table 2-1 provides a list of proactive practices for disease prevention and control and the locations of further information in Chapter 3. Practice Section of Manual for further information Healthy wetland management Wise use of wetlands Site-specific risk assessments ►Section 3. Reactive strategies may include determining an evidence base, conducting surveillance, animal movement restrictions and instigating various other control measures. Reactive strategies for complete disease eradication may involve substantial intervention. With such a wide variety of wetland stakeholders, it is important to appreciate that there is the potential for differences in opinions over reactive disease control strategies and thus cross-cutting education, awareness raising and communication about these activities is advisable, particularly where rapid responses to disease emergence are required. Practice Section of Manual for further information Utilisation of multidisciplinary advisory groups in response to ►Section 3. Their application is illustrated in the case studies throughout the Manual and in the ‘Prevention and Control in Wetlands’ sections of the disease factsheets in Chapter 4. Wetland users do not need to become disease experts but communication and awareness raising programmes should aim to increase motivation to become engaged and ‘do the right thing’, with respect to disease management. This will likely only come from becoming informed about the problem, understanding the issues and implications, and participating in the solutions. Developing capacity to undertake disease management may involve formal education and training of key personnel e. Communication networks of key wetland stakeholders, including disease control authorities, should be established in ‘peacetime’ to facilitate rapid disease control responses should the need arise. This Manual aims to provide some of the information as a foundation for communication and public awareness programmes. The concept of ‘One World One Health’ has arisen due to the appreciation of the fundamental connectivity in health of humans, domestic livestock and wildlife. Embracing an ecosystem approach to health in wetlands involves recognising the dependence of health and well-being on ‘healthy wetlands’ which can only be achieved through wise use, most often at a landscape and/or catchment scale. If wetland stakeholders understand both the impacts of diseases and how to prevent and control them, they will feel motivated and empowered to take action. Stakeholder understanding must be built through effective communications or training but action will also be influenced by capacity to respond. To view disease management as separate to other forms of land and wildlife management ensures that opportunities for good disease prevention will be missed. Therefore, integrating disease management into wetland management means putting disease consideration at the heart of the wetland management planning process. Effective management of any disease is dependent on a good understanding of its epidemiology and the ecology of host populations. The dynamics of disease in wildlife populations can be highly complex, and disease management interventions can have unpredictable outcomes. Invasive alien species and novel pathogens and parasites have many parallels in their biology, the risks they pose, and in the measures required to prevent their establishment and control. Prevention of their introduction is preferable to subsequent control, and wetland management practices aimed at prevention of any of these can provide additional benefits and protection from all. In: Global biodiversity mechanisms: a thematic review of recent developments and future evidence needs.
These findings have been confirmed in further studies that examined the behaviour of orthopaedists [4] buy cheap ampicillin 250 mg line, neurosurgeons [5] and specialists in general [6] ampicillin 250 mg low price, all in the United States of America. Even though litigation generally is settled in favour of the defendant doctors, and remains unusual, the fear of it has a significant impact on the use of imaging. Inappropriate use of imaging is further complicated by the increasing complexity of modern medicine. Clearly, no health care provider can be fully knowledgeable about more than a small area, and best practice can change very quickly. This adds not only intellectual concerns, but also concern about delivering optimal care. This is further complicated by the increasing role that non-physicians, such as physician assistants and other ‘physician extenders’, play in the delivery of care. These factors taken together make a strong argument that imaging is not likely to be optimally utilized, and this has been shown in many studies. In one, for example, it was shown that a large percentage of patients with advanced cancer underwent screening for other cancer [7]. This screening was very likely to have no benefit in terms of longevity or altered treatment. Medical costs have increased dramatically over the last several decades, in many cases in concert with improved care, and it is clear that imaging has provided major advances in health care. Over the past few years, for a number of reasons, there has been increased concern about the exposure of populations and individuals to ionizing radiation. It is essentially impossible to define the individual risks and population risks are also virtually impossible to define with precision. Recent studies, however, have suggested that limited exposure to ionizing radiation does measurably increase the cancer risk for populations [12, 13]. There are, in summary, two important basic concepts that must be kept in mind: first, there is potential risk of exposure to diagnostic level ionizing radiation, so any use should be based on a risk– benefit analysis, with the possible benefits to be gained through the imaging outweighing the theoretical risks of ionizing radiation. Secondly, the concern about the possible adverse effects of radiation can be used to help educate the lay public, to enable them to consider the risk:benefit ratio whenever imaging (particularly using ionizing radiation) is considered. This concern logically leads to the conclusion that there is need for ongoing education and specific guidance in the optimal use of imaging, and this is probably best achieved and most likely to be successful if it is based on methodologically sound, widely accepted guidelines for the use of imaging. It follows, however, that imaging guidelines are likely to be very difficult to develop and deploy, given the complexity of modern medicine and the wide variations in disease patterns, availability of technology and treatments, and knowledge, but they are also necessary. There has been much discussion about how guidelines should be constructed, but there are several areas of wide consensus. First, clinical guidelines should be based to as large an extent as possible on high quality, peer reviewed literature. The available literature, however, is virtually never sufficient to provide data based guidance, except in very limited areas, so any guidelines must be data driven but supplemented by expert opinion. Guidelines must also be based on transparent, well defined, reproducible methodology that indicates how the literature is reviewed and synthesized, and how conclusions are reached. They must be developed and vetted by relevant experts, in this case imaging experts, as well as other health care providers, patients and even payers. They require specific expertise in the topic being addressed, as well as in methodology. Imaging guidelines differ from most other guidelines in that the focus is confined to guiding the ordering health care provider in the best use of imaging. They are, in a sense, horizontal, addressing all imaging, rather than vertical, addressing all aspects of a specific disease. Other widely accepted ones include those from the Royal College of Radiology of the United Kingdom [15], the Canadian Association of Radiologists and the Diagnostic Imaging Pathways from Western Australia [16]. Each panel has 8–20 members, with broad representation geographically and in modality expertise. Non-radiologist societies, such as the American College of Chest Physicians, the Society of Vascular Surgery and the American Society of Neurosurgery, have representatives on the panels. Currently, over 800 topics are addressed by specific appropriateness criteria and variants. Each topic is developed based on a perceived need, due to impact of disease, prevalence, cost implications and potential for impact on care and outcomes, as well as the availability of relevant peer reviewed studies in the published literature. Topics are developed by an assigned author who reviews, categorizes and selects and rates the relevant literature. An evidence table, consisting of the selected publications, is then created, which forms the basis for a narrative on the topic and presents and discusses all of the relevant imaging modalities. First, the panel chair and then the entire panel reviews all of this material, and then each modality in each variant is voted on for appropriateness. This is done using a modified Delphi approach, with three rounds of voting, one or two conference calls and consensus defined as 80% agreement of those voting. Rating is done on a scale of 1–9, with 1–3 defined as ‘usually not appropriate’, 7–9 as ‘usually appropriate’ and 4–6 as ‘may be appropriate’ (Fig.